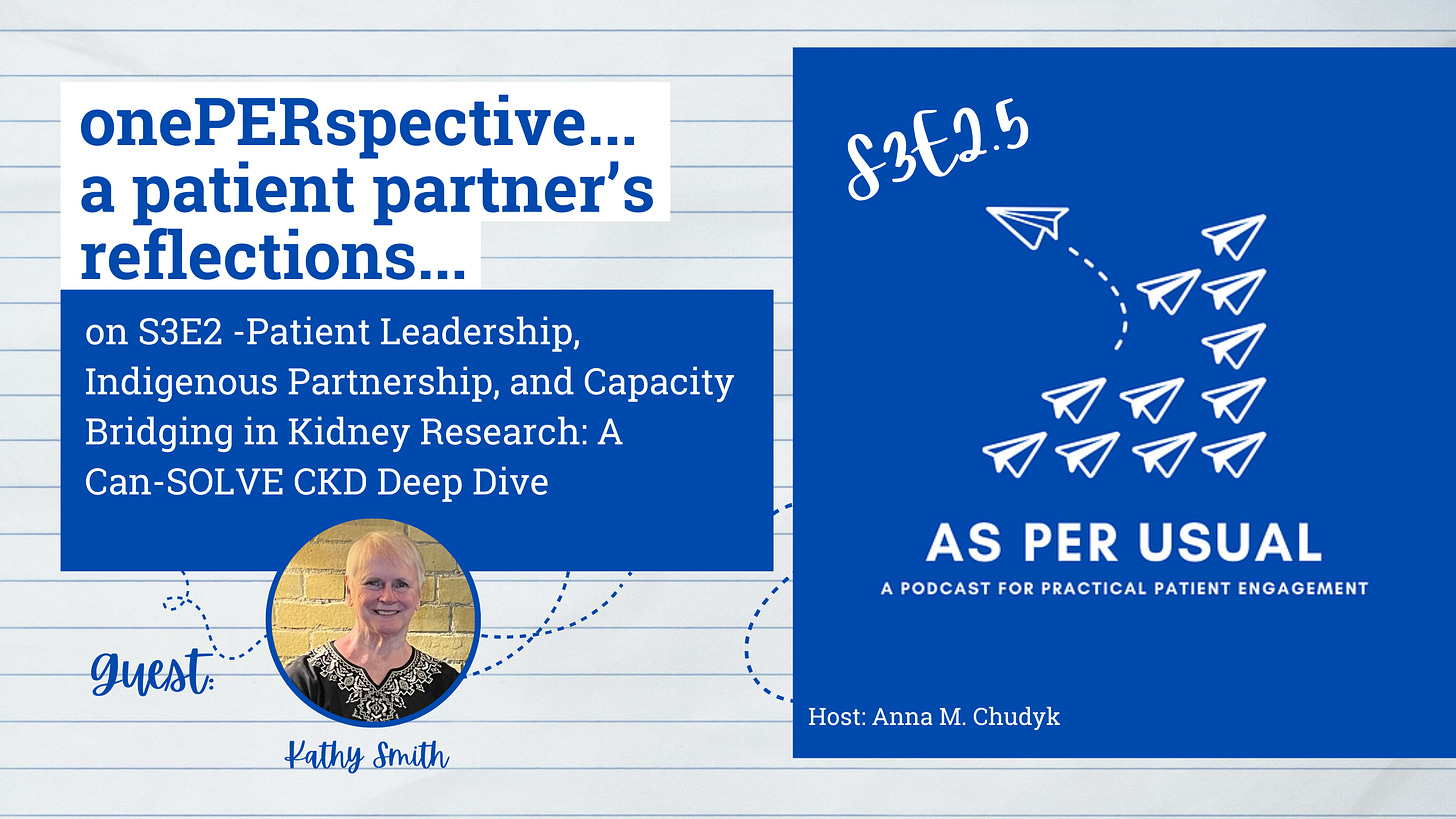
Meet our guest listener
Kathy Smith: Kathy Smith is a cancer survivor and a cancer care partner actively engaged as a co-author in many healthcare research projects - including Anna M. Chudyk’s work on better understanding patient partners’ perspectives on engagement and exploring future directions for Canadian patient-oriented research. She is a patient research/awards reviewer for many organizations including the Canadian Cancer Society.
Episode Transcript:
Anna:
Hi everyone! Welcome to onePERspective - a bi-weekly segment in which patient partner Kathy Smith shares a synopsis and key reflections from the previous episode of asPERusual -- a podcast for practical patient engagement. My name is Anna Chudyk and I am asPERusual’s host. In today’s episode, Kathy will be commenting on S3E2 of asPERusual. In that episode, I sat down with Melanie Talson and Cathy Woods to learn all about patient engagement within the Can-SOLVE CKD Network, which is a Canada-wide network of patients, scientists, and health care professionals devoted to creating innovative kidney care solutions. Alright Kathy, lets turn it over to you and your onePERspective.
Kathy Smith:
Thank you, Anna and hello, everyone. I am speaking to you from the centre of Canada along the shores of Lake Superior, or Gitchigumi, the largest, deepest, coldest and cleanest freshwater lake in the world. I wish to acknowledge that my City of Thunder Bay is situated on the traditional land of the Anishinaabe peoples, including the Ojibwa of Fort William First Nation, signatories to the Robinson Superior Treaty of 1850. I thank our ancestral land keepers for centuries of sustainable stewardship of this beautiful area and for kindly sharing the bounties of this rich land with everyone. I also wish to express my appreciation for the significant contribution of the Metis nation. I am sorry for the mistakes made and mistreatment of Indigenous peoples by colonists in the past and I am committed to working together for truth and reconciliation. Miigwetch.
If ever there was an award for a solid and sustainable engagement strategy, today’s Chronic Kidney Disease (CKD) Px engagement platform would certainly be a strong contender. I am most impressed with how they have integrated the Indigenous voice and with their capacity-building training modules, including bi-directional Capacity Bridging.
Melanie Talson & Cathy Woods from Can-SOLVE CKD: Canadians Seeking Solutions and Innovations to Overcome Chronic Kidney Disease describe their network as a national partnership of lived experience patients; learned experience researchers; laboured experience health care workers and clinicians; and leaders – the managers and policy makers. The four “Ls” work together to transform treatment and care and improve the outcome for those living with debilitating chronic kidney disease.
Can-SOLVE’s tagline is “the right treatment for the right person at the right time and place.” No small task when you consider CKD affects a disproportionate number of Indigenous people many of whom live in remote, even fly-in, communities. That is why I am so impressed to see that this group has a strategy for addressing that barrier to care. Can-SOLVE has an Indigenous-led partner group, IPERC -Indigenous Peoples Engagement and Research Council. IPERC’s focus is on Indigenous kidney care challenges unique to this harder to reach, often underserved, group. Cathy, of the Bear Clan, is a member of Naicatchewenin First Nation in Northwestern Ontario, is the patient partner and a lead researcher of the Kidney Check Research Project which seeks to screen, triage and treat Indigenous people living in rural and remote communities in the three western provinces and British Columbia. Patient partners within both groups prioritize and co-lead research projects like this one, ensuring meaningful and relevant engagement at every stage. Furthermore, there is a Patient Governance Council – a leadership team made up of representatives of both interest groups who decide on plans and policies that affect the entire CKD community.
Our speakers have done a great job describing each of the 6 Rs upon which they built their engagement platform: Respect, Responsibility, Reciprocity, Relevance, Relationships and Realness. Realness is a term I had not heard of in engagement platforms before. But I do understand and appreciate its inclusion. We need to fit our hats to the task as I like to call it. Our real life has given each of us many hats, but which shall we wear to best meet the asks of the task? Patients and providers work best when they find common ground, common interests and common language with lived experience input “as is”. Bring your real, authentic self to the table. Respect for individual differences and perspectives sees real-world impacts.
Equally impactful is how patient partners like Cathy describes her involvement in CANSOLVE as healing, empowering, and deeply purposeful – creating a space for ordinary people to accomplish extraordinary things. As the famous anthropologist, Margaret Mead, phrased it; never doubt that a small group of thoughtful, committed citizens can change the world. It’s the only thing that ever has.”
Finally, I’d like to acknowledge CANSOLVE’s Bridging Capacity. Building capacity is an integral component of patient engagement strategies. Training modules are co-designed to buildup the knowledge and provide the necessary tools for patients to engage in a research project. These helps are unidirectional in scope. So how does Bridging Capacity differ from Building Capacity? Bridging Capacity is bi-directional. Patients and providers both learn from each other. I cant think of a better tool for bridging the power differential and creating strong work relationships!
All in all, CANSOLVE and IPERC have really empowered patients to enhance research relevance to better the outcome for all with chronic kidney disease.
PERsonally Speaking
My three take-aways:
Could this Indigenous Partnership (IPERC) model be used to incorporate the voice of many other underserved populations – the remote; the homeless; the new Canadians? These groups are surely concerned about their health, but they do not want to, or cannot, come to our Table. So, meet them where they are at with separate interest groups run by their own leaders and their own peers. Then the leaders of the various interest groups could come together to form an overarching Senior Team. This makes for a much more inclusive and diverse Patient Engagement Platform!
Capacity Bridging This was a term I had not heard of before but I very much like it for the added emphasis it brings to an engagement platform. This bridging is a bi-directional sharing of knowledge between the lived experience experts and the learned experience experts. It stresses the importance of respecting that all members of the team bring unique experiences and skill sets. This concept guides mentorship, training, and peer review practices across the network. Patient partners are highly valued for their different hats they bring to a task on the TEAM: Together Everyone Accomplishes More. Together is better!
Relationship Building is at the heart and soul of every Patient Engagement Platform. It takes a patience of time and a whole lot of money. It must be accounted for in research budgets and run by a paid, highly trained and skilled multi-tasker manager. Anything less jeopardizes the success of the engagement platform and perhaps the relevance and value of the research itself.
At this time, I would like to thank everyone for the privilege and the opportunity of speaking to you on these podcasts. In particular, I want to do a huge shout out to my heroine, Anna, for including me and asking me to do these podcasts. As Anna is moving forward with the pediatric and youth groups, I want a fresh voice to help her with these podcasts. But in any case, I wish Anna all the best as she goes forward with this labor of love. I can't tell you how much time and effort Anna has shown and the passion that she has dedicated to helping all patients engage meaningfully and relevantly with academic partners in research. Thank you. And happy trails, Anna.
Anna:
Thanks Kathy for this, and all of the other onePERspective’s to date. As you know, your encouraging emails summarizing all you learned from the release of this podcast’s initial episodes were the impetus for creating the onePERspective segment. I’ve really enjoyed hearing your reflections and collaborating with you on the creation of these episodes. Even with all your engagement related jet setting, I could also count on you to come through on your episode… and somehow find the time for it. Big hugs to you and I’m glad we have research we’re collaborating on together so it’s not actually a good bye.
Moving forward this season, I’m going to continue with onePERspective but it’s taking a different twist. A big reason why I have chosen to focus the remainder of season 3’s episodes on engaging children, youth, and families is for my own learning as I expand my research program to focus on these populations. I am currently moving in this direction through a pharmacogenetics study I am collaborating on with my colleague Abdullah Maruf, as well as work I am doing with colleagues to redesign pediatric-to-adult transition care services for youth and families living with congenital heart disease. Sasha Kullman is a talented PhD trainee working under my supervision on the congenital heart disease project. Given her passion and penchant for patient engagement and knowledge translation, I thought that it would be a great opportunity for her to take over onePERspective this season, and offer a trainee perspective on her take-aways from the episodes. She’s very brilliant and I can’t wait to hear her episode takeaways as her insights always make me think.
In the next full episode of asPERusual, I kick off the rest of this season’s focus on how to meaningfully engage children, youth, and families in health research. Guests Brianna Hunt, Onalee Garcia-Alecio, and Michelle Roy, will share their experience with engaging in the iCARE study—Canada’s largest cohort of youth with type 2 diabetes. We’ll also discuss what makes engagement meaningful over time, the value of lived experience, and practical tips for involving youth and families in ways that are inclusive, trauma-informed, and fun. The episode is going to drop on April 28th so be sure to check it out by visiting our website asperusual.substack.com or wherever it is that you download your other podcast episodes from. If you do visit the website, be sure to check out the interactive transcript from this, and other episodes, as well as to subscribe to the podcast’s newsletter! As always, you can reach me by emailing anna.asperusual@gmail.com or by adding me to LinkedIn by searching Anna M. Chudyk – CHUDYK.
Until next time, thanks again for tuning in and let’s keep working together to make patient engagement the standard, or asPERusual.











Share this post